By Peter D’Auria/VTDigger
Vermont hospitals are seeking the Green Mountain Care Board’s permission to increase commercial insurance charges and their revenue from patients, an annual process that comes amid widespread concern over hospitals’ financial health.
Each year, hospitals request increases for the next fiscal year in their net patient revenue — revenue brought in by caring for patients — and in how much they can bill commercial insurance companies for that care. The Green Mountain Care Board, a key health care regulator, can sign off on those requests, or allow smaller increases.
The board sets non-binding benchmarks to signal their goals for hospital budgets. For patient revenue, the benchmark — 3.5% growth — is based on state health care reform goals. The commercial insurance price benchmark — 3.4% growth — is based on medical inflation indices, according to Green Mountain Care Board chair Owen Foster.
“As we are all deeply familiar, our hospitals have been under great pressure over the last few years, and intensely understand the pressures facing Vermonters and the health care delivery systems,” Vermont Association of Hospitals and Health Systems president and CEO Mike Del Trecco said at a Green Mountain Care Board hearing Wednesday, Aug. 7.
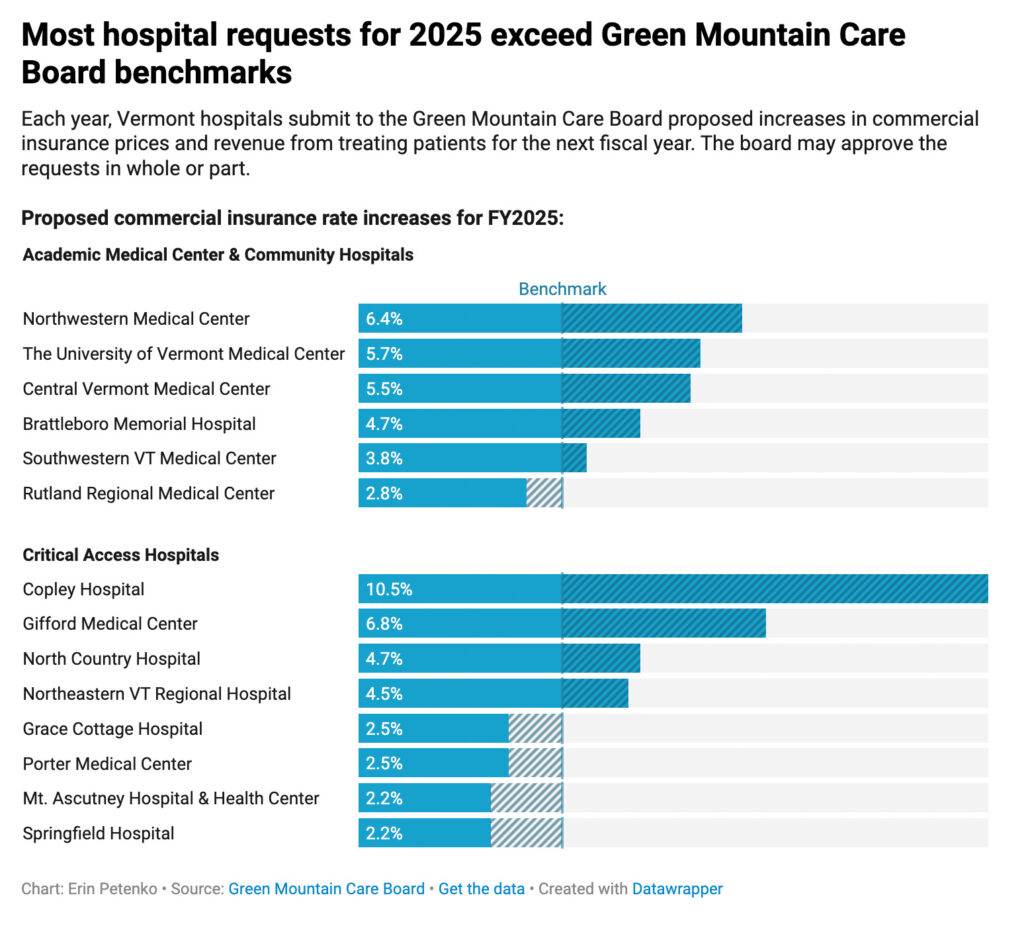
– Chart shows the proposed commercial insurance rate increases for fiscal year 2025.
Most hospitals in the state are operating in the red, and many Vermonters are struggling to access the care they need. Wait times for procedures are long, medical staff are in short supply, and, because of a lack of long-term care facilities, hospitals are often left caring for patients that no longer need to be there but have nowhere else to go — among a litany of other problems.
Mike Fisher, Vermont’s chief health care advocate, told board members last Wednesday that Vermont is facing “a perfect storm” in the realm of health care.
“We think it’s important to remain focused on what you can do to really address, as I said, the storm in front of us,” he said. “And that is hospital prices and hospital costs.”
This year, requests varied widely among the 14 hospitals, but most exceed the benchmarks set by the board.
On the low end of the range, Springfield Hospital and Windsor’s Mt. Ascutney Hospital and Health Center are seeking to increase their commercial insurance charges by only 2.2%, according to data compiled by the Green Mountain Care Board.
Morrisville’s Copley Hospital, meanwhile, is seeking to increase its commercial insurance charges by 10.5%.
“Copley’s biggest challenge in its rate request, is our inability to charge a fair and reasonable price for basic services provided to Vermonters,” the hospital said in a filing with the Green Mountain Care Board. “Our prices have not kept up with the hospital marketplace in Vermont, and we are spending down our reserves and chipping away at our financial viability at a concerning rate.”
Copley also requested an unusual mid-year rate increase from the Green Mountain Care Board earlier this year, which the board granted after reducing its size.
Requests to increase patient revenue — which rises when hospitals treat more patients, offer new or different services, or insurers pay more — were similarly varied.
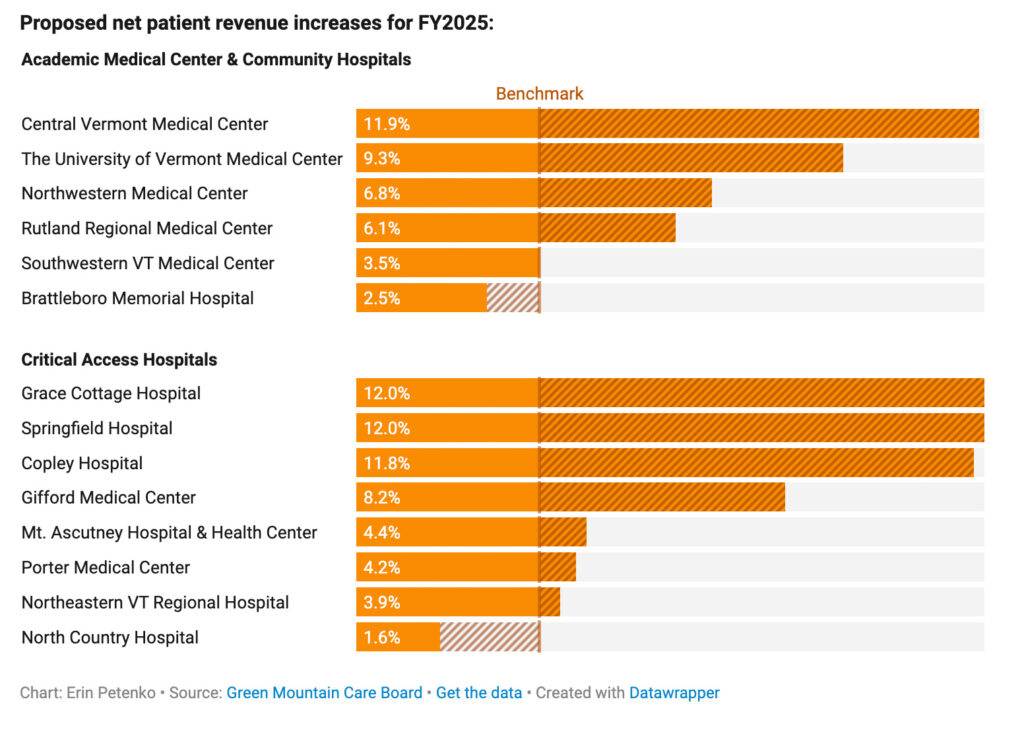
– Chart shows the proposed net patient revenue increases for fiscal year 2025.
Newport’s North Country Hospital, for example, is requesting just a 1.6% increase in patient revenue. Springfield and Grace Cottage Hospital, in Townshend, meanwhile, are requesting increases of 12% in patient revenue.
In fiscal year 2025, Springfield Hospital “will focus on continuing to improve our financial stabilization and rebuild volume,” the hospital, which emerged from bankruptcy proceedings several years ago, said in a filing with the care board. “We will focus on identified core services and work to recapture utilization that is currently leaving our service area and, in many cases, leaving Vermont with less convenience for patients and higher cost.”
Some Vermont hospitals — the University of Vermont Medical Center, Porter Medical Center, Northeastern Vermont Regional Hospital and Rutland Regional Medical Center — actually brought in more revenue in fiscal year 2023 than the care board had allowed.
Those overages will be factored into the board’s deliberations as it decides how to handle hospitals’ requests for more revenue and higher costs, Foster, the board chair, said in an interview.
The care board’s decisions must take into account the interconnectedness of Vermont’s health care system, Foster said. Increases in hospital revenue and rates fall on the shoulders of commercial insurance companies, primarily Blue Cross and Blue Shield of Vermont, which covers roughly a third of the state.
And when insurers pay hospitals more, they then need to increase premium prices to cover their own costs. Blue Cross Blue Shield, where administrators say reserves are reaching dangerously low levels, is currently seeking to do exactly that.
Those increases then fall on Vermont businesses and individuals, who pay those premiums.
All in all, this year’s requests were broadly in line with requests in previous years, Foster said. Care board members will consider the requests and issue decisions for each hospital before October 1.
“Now we’ve got to make decisions, and we look to a number of factors,” Foster said. “One is, what’s the hospital’s position financially? Like, how are they doing? Another is the affordability side — like, what will this do to rates, and can people afford it, and how does this align with the state’s goals of affordable health care?”




